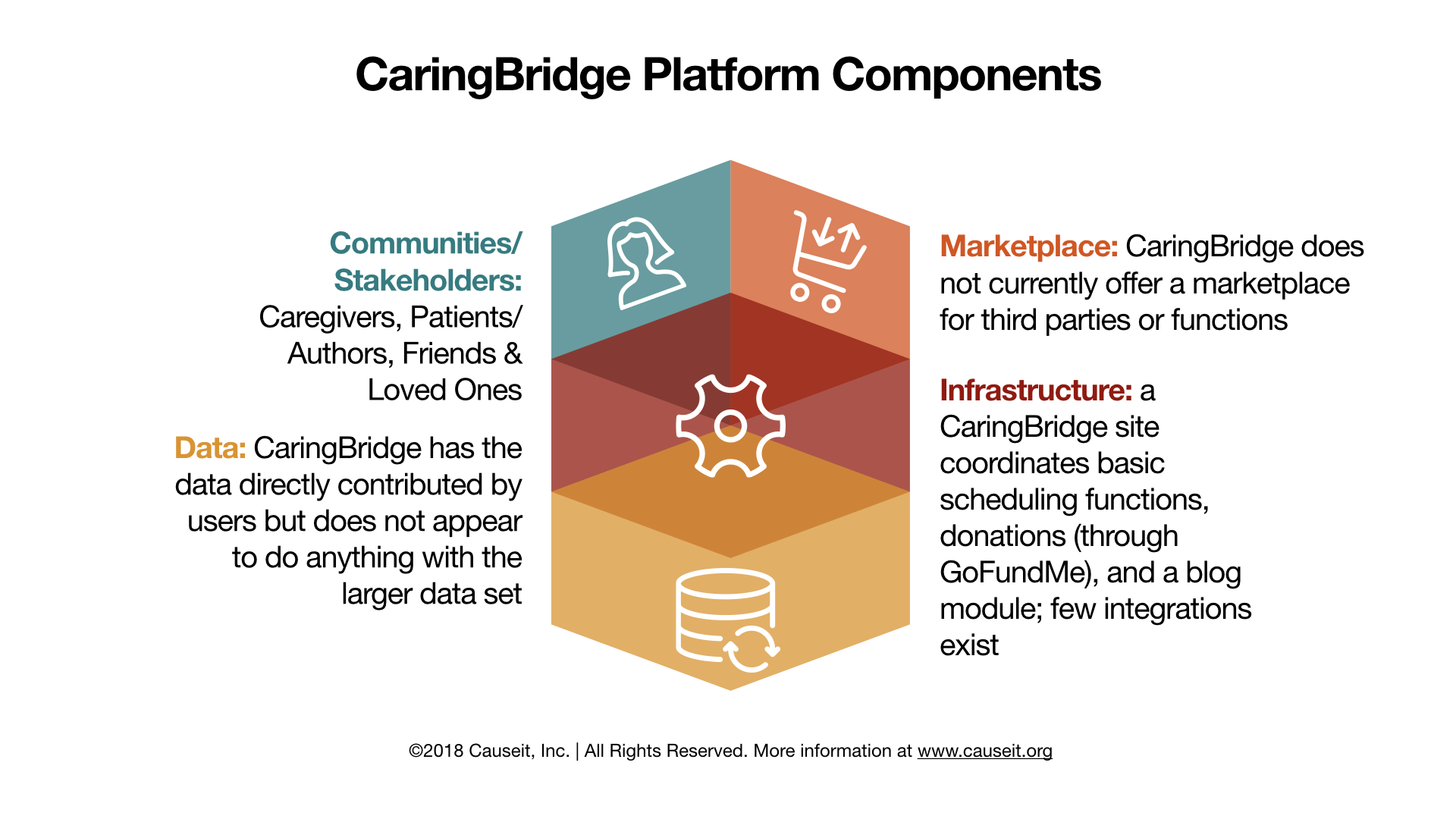
CaringBridge is a simple community site designed to give people experiencing a health crisis a central place to inform family and friends about what is going on and coordinate community care (think dropping off casseroles and giving rides to the doctor). Importantly, the site also serves the needs of caregivers, especially primary caregivers like spouses or a child’s parents, as they try to coordinate charitable offers of help with the complex realities of serious healthcare. The site was started when the founder, Sona Mehring, used her background in software to help friends share information about their premature baby. CaringBridge focuses primarily on basic community functions and some simple onboarding. But it perhaps has struggled to raise its profile because its business model is not clear and it is not sufficiently distinct from the existing hodgepodge of social media sites, direct messaging and calendaring apps, apart from being ad-free. A huge opportunity exists to connect CaringBridge or functions like it with larger patient bases so that doctors become more familiar with it and integrate it with professional caregiving efforts. Right now, the use case remains focused on a specific portion of a larger care plan—the lay caregiver. While important, it may not be as powerful as it could be with deeper integrations.
Stories of caregivers
CaringBridge provides stories from caregivers to inspire and educate each other
Stories on Well-Being and Healing
Stories on well-being & healing: CaringBridge provides stories on well-being and healing to inspire and inform members
Stakeholders
Caregivers
Caringbridge provides a central place for caregivers to keep friends and loved ones apprised of a complex a health journey and to coordinate offers of help with tangible needs, like rides to medical appointments
Patient/Author
Patients and caregivers can both share stories and other updates from their health journey
Loved Ones & Friends
Loved ones and friends can read content posted by others on the site, as well as volunteer for specific tasks; they can also subscribe to notifications so they are always up to date
Citations
- Caringbridge.org
- https://www.caringbridge.org/assets/ugc/content/2016AnnualReportFinalweb.pdf
- Images: caringbridge.org